WHO has raised alarms over India’s weak regulation of medicines following the deaths of children due to adulterated cough syrups. It warned of a ‘regulatory gap’ in screening for toxic chemicals.
The World Health Organization (WHO) has expressed deep concern over the tragic deaths of children in India linked to adulterated cough syrups. In a statement, it flagged a ‘regulatory gap’ in India’s oversight of medicines, especially the failure to routinely screen for toxic chemicals like diethylene glycol (DEG) and ethylene glycol (EG). It urged Indian authorities to thoroughly investigate the source of contamination and to trace any affected pharmaceutical material in circulation.
WHO also called attention to a wider risk, even if the contaminated syrups were not officially exported, they could enter other countries through unregulated channels. The agency stressed it is ready to assist national authorities with investigations and corrective measures, according to a report in Reuters.
What led to the cough syrup tragedy
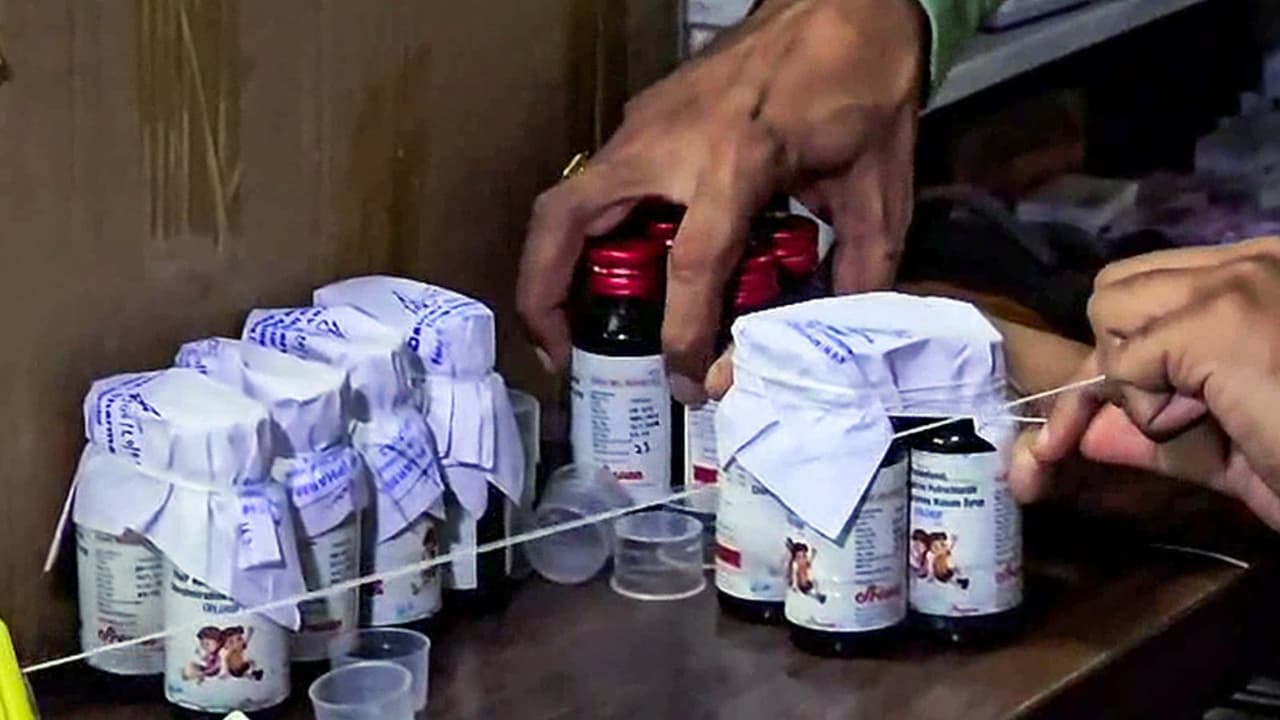
In Madhya Pradesh and Rajasthan, reports emerged of at least 20 children, mostly under age five, dying from kidney failure after being given cough syrup. Many of these deaths were linked to Coldrif cough syrup, manufactured by Sresan Pharmaceuticals. Tests revealed that samples contained an alarming 48.6 percent diethylene glycol, far exceeding thesafe limits.
India’s drug regulator Central Drugs Standard Control Organisation, CDSCO, confirmed that two other syrups, namely Respifresh TR and ReLife, also tested positive for DEG contamination. All three products were immediately recalled, and production has been ordered to halt. Importantly, CDSCO has told WHO that none of these products had been exported.
What WHO is asking and offering
WHO’s primary concerns and recommendations include:
- Ensuring rigorous screening of medicines (both raw materials and finished products) for DEG and EG before they are sold domestically
- Tracing the origin of contamination — to find out whether industrial-grade or impure chemicals were used
- Identifying and removing contaminated stock still circulating in the market
- Being vigilant about the risk of export of tainted medicines through unofficial routes
- Offering technical support and guidance to Indian regulators and agencies to strengthen oversight
WHO has reached out to the CDSCO and urged clarity on export status and inspection protocols.
Previous syrup scandals
This is not the first time Indian-made syrups have caused international health scares. In 2022, dozens of children died in The Gambia after consuming cough syrups traced back to Indian manufacturers. In another case, toxic syrups caused fatalities in Uzbekistan. Those incidents prompted WHO medical alerts and pushed India to mandate stricter testing for syrups destined for export.
However, critics argue that prior rules applied more strictly to exported syrups than to those sold domestically. The current tragedy underscores how domestic market oversight has remained weak. The Indian Express +2 Vision IAS +2
India’s action so far
In response to the public outcry and WHO’s caution, Indian authorities have taken immediate steps:
- CDSCO has issued urgent alerts to all states, instructing them to ensure testing at every stage, from raw material to finished product, before release.
- States and union territories have been asked to monitor manufacturers for compliance and to maintain strict records of tests. The Times of India
- The owners of Sresan Pharmaceuticals (maker of Coldrif) have been arrested and legal steps are underway.
- Several state drug regulators have pulled affected batches from shelves and issued warnings to medical outlets.
- The regulator has also emphasised that both active and inactive ingredients (excipients) must be tested before use in production.
DCGI orders strict testing of raw materials and medicines
In response to the tragedy, the Drugs Controller General of India (DCGI) has issued a strong directive to all States and Union Territories, urging them to strictly follow the Drugs and Cosmetics Rules, 1945.
In a letter dated October 7, DCGI Dr. Rajeev Singh Raghuvanshi underlined the critical need for thorough testing of all raw materials, including active ingredients and excipients, before they are used in the production of medicines. He said that both raw materials and finished pharmaceutical formulations must be carefully tested to ensure safety and quality.
The DCGI also reminded drug manufacturers and testing laboratories that no shortcuts or assumptions can be made while handling materials used in pharmaceutical production. Every batch, he stressed, must be verified to prevent any chance of contamination or impurity.
This direction aims to close the regulatory gaps exposed by the recent deaths linked to adulterated cough syrups and to strengthen India’s overall drug safety framework.
Why the regulatory gap is alarming
1. Weakness in screening protocols
Many pharmaceutical units lack advanced testing capability. While gas chromatography is effective in detecting DEG contamination, many smaller firms rely on less reliable methods. Experts say regulators should require stronger testing standards for all manufacturers.
2. Inconsistent domestic vs export scrutiny
Previously, only syrups meant for export underwent rigorous testing in central government labs. Domestic syrups often escaped such scrutiny, creating a blind spot. The tragedy shows the cost of that gap.
3. Vulnerable supply chains
Contamination can originate at raw material suppliers. If industrial-grade chemicals are mixed into what should be pharmaceutical-grade materials, entire batches may become unsafe. Unless regulators inspect the upstream supply chain, risk remains.
4. Risk of international spread
Even if the contaminated syrups were not officially exported, WHO warns they might slip into foreign markets through parallel trade or smuggling, especially in countries with weak import oversight.
What must be done going forward
To prevent such tragedies, India (with WHO support) must:
- Mandate universal screening for DEG and EG in all pharmaceutical products, regardless of whether they are for domestic or export markets
- Ensure all manufacturing units have or use labs capable of detecting contaminants (e.g. by gas chromatography)
- Enforce strict vendor qualification rules so raw materials come only from trusted sources
- Strengthen regulatory inspections, with unannounced audits and independent third-party validation
- Issue medical product alerts internationally if contaminated medicines are suspected of crossing borders
- Set up a publicly accessible database listing drug recalls, lab test results, and manufacturer compliance
- Impose strong legal penalties on companies and individuals responsible for negligence or fraud
The WHO’s warning brings to light a harsh reality: India’s regulatory framework for medicines has serious gaps, especially in ensuring safety of products sold within the country. The tragedy of children dying from contaminated cough syrup is a wake-up call not just for India but for all nations relying on Indian pharmaceutical exports. With WHO support and determined reform, India can strengthen its systems, regain public trust, and protect lives.
(With ANI inputs)