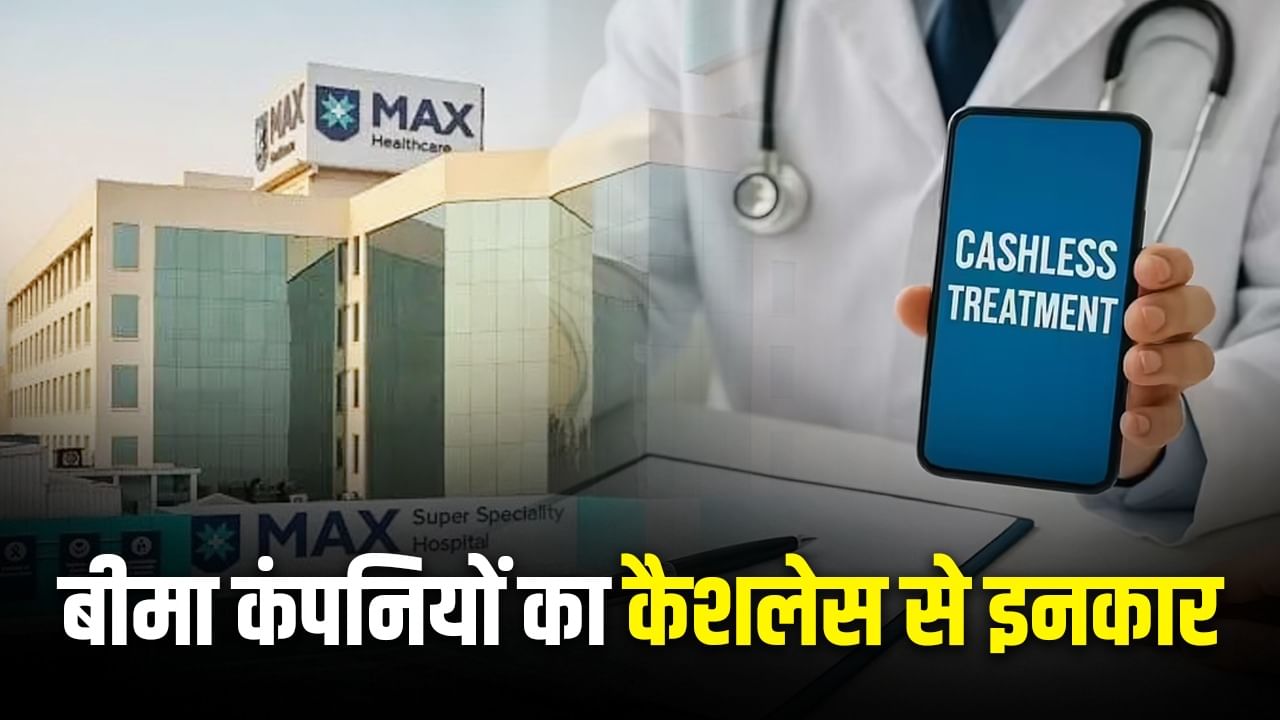
People undergoing treatment through health insurance at Max Hospital have suffered a big setback. Niva Bupa, Star Health and Care Health Insurance have discontinued cashless facilities from Max Hospital across India. These companies have said that cashless medical treatment will not be provided in any branch of Max Hospital in any branch across the country. Earlier, the hospital had announced to stop the cashless facility of Bajaj Allianz.
Companies have said that if treatment has to be done in this hospital, then insurance holders can take reimbursement facility. The office claim team will reimbursement of the hospitalization. Insurance companies have said that the papers required for reections include discharge summer, all reports, all prescriptions and doctors notes, all bills, Aadhaar cards, PAN cards and checks.
Hospital stopped cashless service of these companies
Two days ago, AHPI, an organization of hospitals AHPI, directed all the members hospitals to stop the cashless treatment facility of Bajaj Aaliyanz General Insurance from 1 September. This includes more than 20,000 hospitals including Max Super Specialty and Fortis escorts. A similar notice was also sent to Care Health Insurance. AHPI has sought a reply from Care Health till 31 August. If the answer is not received, the cashless facility will also be closed for the policy holders of the care. If this applies, then patients with Bajaj Aaliyanj or Care’s insurance policy will have to pay the hospital expenses first and later the insurance company will rebel.
After all, what was the matter?
AHPI Director General Dr. Girdhar Gyani had said that medical expenses in India are increasing at the rate of 7-8% every year. This includes staff salary, medicines, medical goods, electricity-water and other expenses. Hospitals try their best to reduce the expenditure, but it is not possible to treat at the old rate. If this continues, the care of the patients will be affected, which AHPI and its members cannot approve the hospital. According to AHPI, Bajaj Aaliyanz has been rejecting the demand to change the treatment rates every 2 years and talks about reducing the reverse rate. At the same time, hospitals allege that Bajaj Aaliyanz delays claim settlement and patients also get discharge approval late.