Scientists uncover a molecular “switch” in lung cells that controls repair vs. defense. Targeting it could boost tissue regeneration and treat chronic lung diseases.
Scientists at Mayo Clinic have discovered a molecular “switch” in the lungs that determines whether lung cells focus on repairing tissue or fighting infection — a finding that could revolutionize treatments for chronic lung diseases.
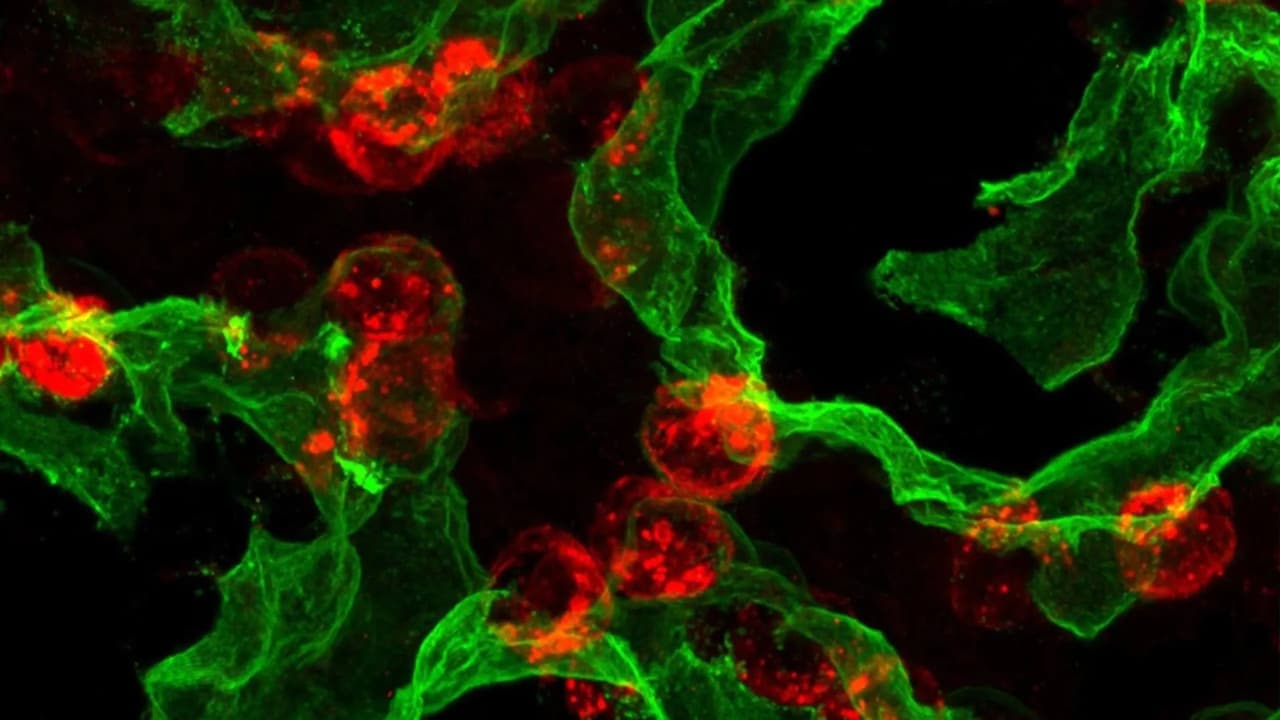
The study, published in Nature Communications, focused on alveolar type 2 (AT2) cells, specialized lung cells that both protect the lungs and act as reserve stem cells. AT2 cells produce proteins that keep air sacs open for breathing and regenerate alveolar type 1 (AT1) cells, which enable oxygen exchange.
How the Lungs Repair Themselves
AT2 cells are unique because they play a dual role: defending the lungs against infection while also serving as stem cells to rebuild damaged tissue. This dual function explains why lung repair is often slower in diseases like pulmonary fibrosis, chronic obstructive pulmonary disease (COPD), and after severe viral infections.
Tracking the Life Cycle of Repair Cells
Using advanced imaging, single-cell sequencing, and preclinical models, researchers mapped the “life history” of AT2 cells. They discovered that new AT2 cells remain flexible for about one to two weeks before permanently adopting a specialized function.
The Molecular Clamp That Controls Regeneration
This transition is controlled by a molecular circuit involving three key regulators: PRC2, C/EBPα, and DLK1. One protein, C/EBPα, acts as a clamp that prevents AT2 cells from behaving like stem cells.
“This clamp explains why lung cells can’t repair tissue and fight infection simultaneously,” said Dr. Douglas Brownfield, senior author. “By uncovering this switch, we can start thinking about how to restore balance when it breaks down in disease.”
Why Infections Block Lung Healing
The same molecular switch also determines whether AT2 cells repair tissue or fight infection. This helps explain why infections often slow lung recovery or worsen chronic lung disease. The discovery opens doors for regenerative medicine. Drugs that fine-tune C/EBPα activity could help AT2 cells rebuild tissue, reduce scarring in pulmonary fibrosis, and improve recovery after severe infections.
Looking Ahead: Restoring Lung Function in the Lab
Beyond potential drug therapies, the findings may help identify early disease markers, offering opportunities for preemptive treatments before organ failure occurs. Mayo Clinic researchers are now exploring ways to release the clamp in human AT2 cells, grow them in the lab, and develop cell-based therapies to restore lung function.