New Delhi: For the first time, a kidney has been successfully transplanted into a human after being converted from blood type A to blood type O, the universal donor, using enzymes developed by researchers from the University of British Columbia. A paper describing the advancement has been published in Nature Biomedical Engineering. The technology prevents mismatch and rejection of donor organs. The transplant was conducted on a brain-dead recipient with consent from the family, allowing scientists to observe the immune response to the transplanted organ without risk to the patient. The kidney functioned nominally for two days.
Hyperacute rejection is a rapid immune reaction that can destroy a donor organ within minutes. There was no signs of hyperacute rejection for the first two days. Some blood-type markers reappeared on the third day and triggered a mild reaction, but the damage was not as severe as a typical mismatch. Researchers saw signs indicating that the body was tolerating the organ. The experiment, the first conducted on a human model, allows scientists to improve the long-term outcomes of the procedure. The advancement was the result of over a decade of work, with the researchers looking for a way to strip away the sugars that define blood types since the early 2010s.
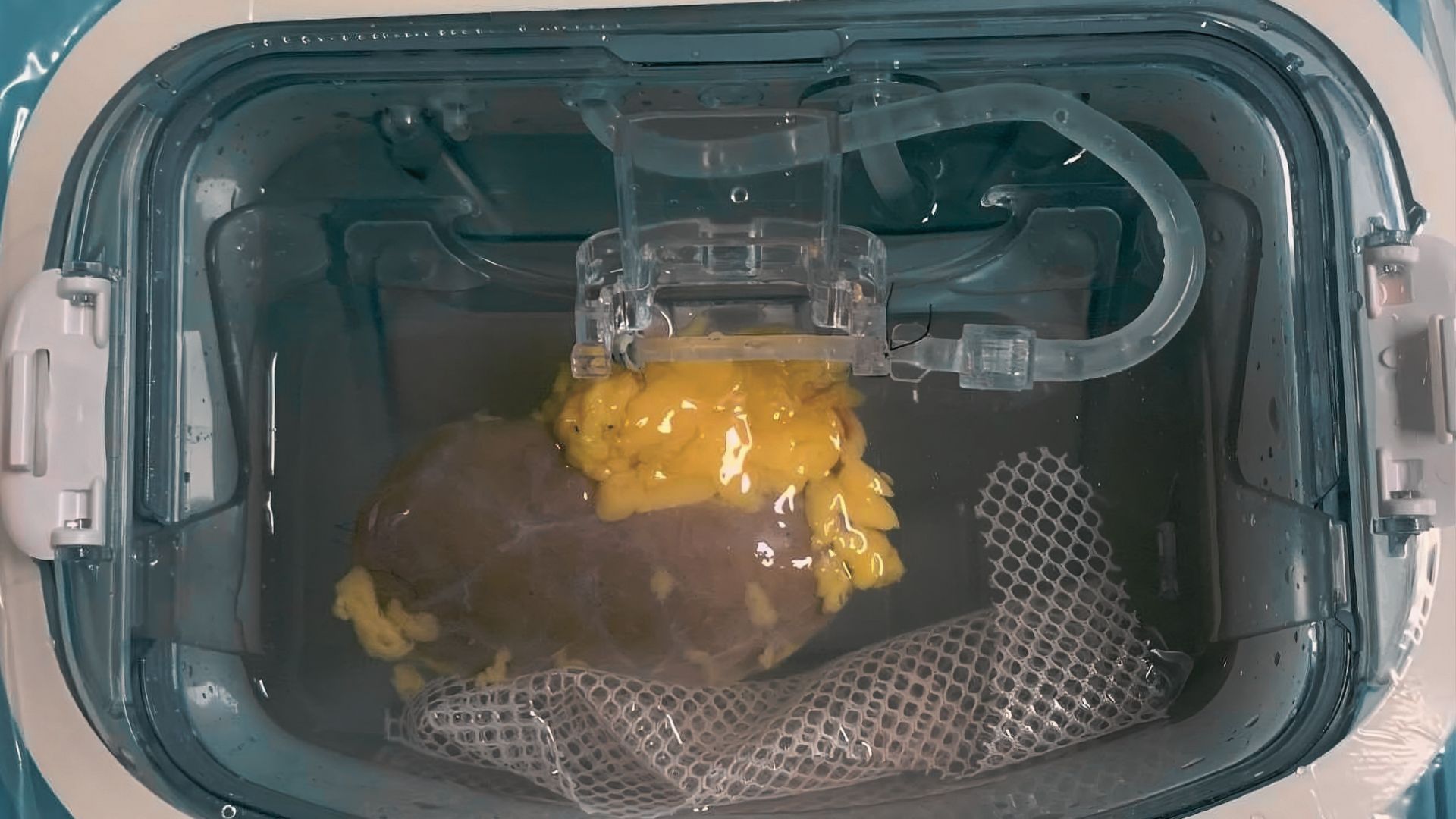
Changing the blood types of donor organs
The sugars or antigens coat the blood vessels of organs. If a recipient’s immune system detects the wrong antigen, it attacks. Type-O patients can only receive type-O organs, that are universally compatible. As a result, type-O patients typically wait between two and four years for a kidney, and can die waiting. Alternative methods to overcome blood-type incompatibility require days of intensive treatments and suppression of the recipient’s immune system, and require organs from living donors. The new approach allows transplants to be performed faster with fewer complications. The technology has previously been demonstrated on lungs.